Shigella Gastroenteritis (Child)
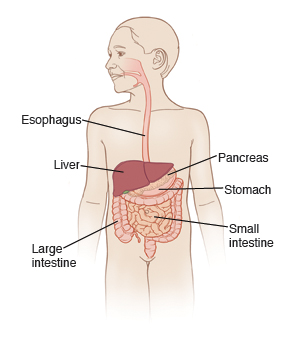
Shigella is an infection of the intestinal tract. It is caused by bacteria. It's more serious than common gastroenteritis (stomach flu) caused by a virus. Shigella infections cause loose watery stools (diarrhea). Stools might be bloody. Your child may have abdominal pain and cramping. Other symptoms of shigella infection include nausea, vomiting, and fever.
Shigella is very contagious. It is easily spread in daycare centers and among household members. The bacteria are passed in the stool. Other children and adults may be infected if they touch anything exposed to the diarrhea of the infected child and then touch their nose or mouth. This could be diapers, clothing, toys, toilets, or food. Once the bacteria are on a child's hands, they can get into their mouth or nose. This will cause infection. This makes good hand washing key to preventing spread of the illness.
Illness starts 2 to 4 days after exposure. It may last 1 to 2 weeks if untreated. It is diagnosed with a stool culture. It may take several days to get the culture results. Antibiotics are sometimes used to treat this type of infection. Your child's healthcare provider will advise you if your child needs antibiotics. Your child will likely feel better within 1 week of treatment. However, shigella bacteria remain in the stool up to 4 weeks after the symptoms are gone. The infection can still be passed to others during that time.
The main danger from this illness is dehydration. This is the loss of too much water and minerals from the body. When this occurs, your child's body fluids must be replaced. This can be done by giving your child oral rehydration solution. Oral rehydration solution is available at pharmacies and most grocery stores. In more severe cases, your child may need treatment for dehydration in the hospital. Do not give sports drinks because they may contain too much sugar and not enough electrolytes.
Home care
Follow all instructions given by your child’s healthcare provider.
If giving medicines to your child:
-
Don’t give over-the-counter diarrhea medicines unless your child’s provider tells you to.
-
If antibiotics were prescribed, make sure your child takes them every day until they're finished or you are told to stop, even if your child feels better.
-
Use other medicine as prescribed. Unless told otherwise, you can give your child acetaminophen or ibuprofen to control pain and fever. Don’t give aspirin or products that contain aspirin to anyone younger than age 19 during times of illness. This may cause liver or brain damage due to a life-threatening condition called Reye syndrome.
-
Your child's provider may prescribe an oral antiemetic medicine if vomiting continues despite a change in diet.
To prevent the spread of illness:
-
Washing hands with soap and clean, running water or using a hand sanitizer is the best way to prevent the spread of infection. Wash your hands before and after caring for your sick child.
-
Wash your hands after changing diapers or cleaning up after your child
-
Clean the toilet after each use. Then wash your hands.
-
Keep your child out of daycare until your child's provider says it's OK to go back.
-
Wash your hands before, during, and after preparing food. Keep in mind that people with diarrhea or vomiting should not prepare food for others.
-
Wash your hands after using cutting boards, countertops, and knives that have been in contact with raw foods.
-
Keep uncooked meats away from cooked and ready-to-eat foods.
-
Teach all people in your home how to wash their hands:
-
Wet your hands with clean running water. Lather the backs of your hands, between your fingers, and under your nails.
-
Scrub your hands for at least 20 seconds. This is about how long it takes to hum the "Happy Birthday" song 2 times.
-
Rinse your hands well and dry them with a clean towel.
Giving liquids and food
The main goal while treating vomiting or diarrhea is to prevent dehydration. This is done by giving your child small amounts of liquids often.
-
Keep in mind that liquids are more important than food right now. Give your child small amounts of liquids at a time, especially if the child is having stomach cramps or vomiting.
-
For diarrhea. If you're giving milk to your child and the diarrhea isn't going away, stop the milk. In some cases, milk can make diarrhea worse. If that happens, use oral rehydration solution instead. Do not give apple juice, soda, sports drinks, or other sweetened drinks. Drinks with sugar can make diarrhea worse.
-
For vomiting. Start with oral rehydration solution at room temperature. Give 1 teaspoon (5 ml) every 5 minutes. Even if your child vomits, continue to give oral rehydration solution. Much of the liquid will be absorbed, despite the vomiting. After 2 hours with no vomiting, start with small amounts of milk or formula and other fluids. Increase the amount as tolerated. Don't give your child plain water, milk, formula, or other liquids until vomiting stops. As vomiting decreases, try giving larger amounts of oral rehydration solution. Space this out with more time in between. Continue this until your child is making urine and is no longer thirsty (has no interest in drinking). After 4 hours with no vomiting, restart solid foods. After 24 hours with no vomiting, resume a normal diet.
-
You can resume your child's normal diet over time as they feel better. Don’t force your child to eat, especially if they're having stomach pain or cramping. Don’t feed your child large amounts at a time, even if they're hungry. This can make your child feel worse. You can give your child more food over time if they can tolerate it. Foods you can give include cereal, mashed potatoes, applesauce, mashed bananas, crackers, dry toast, rice, oatmeal, bread, noodles, pretzels, soups with rice or noodles, and cooked vegetables.
-
If the symptoms come back, go back to a simple diet or clear liquids.
Follow-up care
Follow up with your child’s healthcare provider, or as advised. If a stool sample was taken or cultures were done, call the provider for the results as instructed.
Call 911
Call 911 if your child has any of these symptoms:
When to get medical advice
Call your child’s healthcare provider or get medical care right away if any of these occur:
-
Symptoms get worse after 3 days of treatment
-
Diarrhea lasts more than 1 week while on antibiotics
-
More than 8 diarrhea stools within 8 hours
-
Belly pain that gets worse
-
Constant lower right belly pain
-
Repeated vomiting after the first 2 hours on liquids
-
Occasional vomiting for more than 24 hours
-
Continued severe diarrhea for more than 24 hours
-
Blood in vomit or stool
-
Drinking less
-
Signs of dehydration. These include very dark urine, no urine for 8 hours, no tears when crying, sunken eyes, or dry mouth
-
Fussiness or crying that can't be soothed
-
-
New rash
-
Fever (see Fever and children, below)
Shigella often causes a fever. Unless advised otherwise by your child's healthcare provider, call your provider right away based on these guidelines:
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 months, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older